Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women receiving prophylactic oxytocin: a double-blind, randomised, non-inferiority trial
Abstrak (ringkasan)
Oxytocin, the gold-standard treatment for post-partum haemorrhage, needs refrigeration, intravenous infusion, and skilled providers for optimum use. Misoprostol, a potential alternative, is increasingly used ad hoc for treatment of post-partum haemorrhage; however, evidence is insufficient to lend support to recommendations for its use. This trial established whether sublingual misoprostol is non-inferior to intravenous oxytocin for treatment of post-partum haemorrhage in women receiving prophylactic oxytocin. In this double-blind, non-inferiority trial, 31 055 women exposed to prophylactic oxytocin had blood loss measured after vaginal delivery at five hospitals in Burkina Faso, Egypt, Turkey, and Vietnam (two secondary-level and three tertiary-level facilities). 809 (3%) women were diagnosed with post-partum haemorrhage and were randomly assigned to receive 800 μg misoprostol (n=407) or 40 IU intravenous oxytocin (n=402). Providers and women were masked to treatment assignment. Primary endpoints were cessation of active bleeding within 20 min and additional blood loss of 300 mL or more after treatment. Clinical equivalence of misoprostol would be accepted if the upper bound of the 97.5% CI fell below the predefined non-inferiority margin of 6%. All outcomes were assessed from the time of initial treatment. This study is registered with ClinicalTrials.gov, number NCT00116350. All randomly assigned participants were analysed. Active bleeding was controlled within 20 min after initial treatment for 363 (89%) women given misoprostol and 360 (90%) given oxytocin (relative risk [RR] 0.99, 95% CI 0.95-1.04; crude difference 0.4%, 95% CI -3.9 to 4.6). Additional blood loss of 300 mL or greater after treatment occurred for 139 (34%) women receiving misoprostol and 123 (31%) receiving oxytocin (RR 1.12, 95% CI 0.92-1.37). Shivering (152 [37%] vs 59 [15%]; RR 2.54, 95% CI 1.95-3.32) and fever (88 [22%] vs 59 [15%]; 1.47, 1.09-1.99) were significantly more common with misoprostol than with oxytocin. Six women had hysterectomies and two women died. Misoprostol is clinically equivalent to oxytocin when used to stop excessive post-partum bleeding suspected to be due to uterine atony in women who have received oxytocin prophylactically during the third stage of labour. The Bill & Melinda Gates Foundation.
Headnote
Summary
Background Oxytocin, the gold-standard treatment for post-partum haemorrhage, needs refrigeration, intravenous infusion, and skilled providers for optimum use. Misoprostol, a potential alternative, is increasingly used ad hoc for treatment of post-partum haemorrhage; however, evidence is insufficient to lend support to recommendations for its use. This trial established whether sublingual misoprostol is non-inferior to intravenous oxytocin for treatment of post-partum haemorrhage in women receiving prophylactic oxytocin.
Methods In this double-blind, non-inferiority trial, 31 055 women exposed to prophylactic oxytocin had blood loss measured after vaginal delivery at five hospitals in Burkina Faso, Egypt, Turkey, and Vietnam (two secondary-level and three tertiary-level facilities). 809 (3%) women were diagnosed with post-partum haemorrhage and were randomly assigned to receive 800 μg misoprostol (n=407) or 40 IU intravenous oxytocin (n=402). Providers and women were masked to treatment assignment. Primary endpoints were cessation of active bleeding within 20 min and additional blood loss of 300 mL or more after treatment. Clinical equivalence of misoprostol would be accepted if the upper bound of the 97.5% CI fell below the predefined non-inferiority margin of 6%. All outcomes were assessed from the time of initial treatment. This study is registered with ClinicalTrials.gov, number NCT00116350.
Findings All randomly assigned participants were analysed. Active bleeding was controlled within 20 min after initial treatment for 363 (89%) women given misoprostol and 360 (90%) given oxytocin (relative risk [RR] 0.99, 95% CI 0.95-1.04; crude difference 0.4%, 95% CI -3.9 to 4.6). Additional blood loss of 300 mL or greater after treatment occurred for 139 (34%) women receiving misoprostol and 123 (31%) receiving oxytocin (RR 1.12, 95% CI 0.92-1.37). Shivering (152 [37%] vs 59 [15%]; RR 2.54, 95% CI 1.95-3.32) and fever (88 [22%] vs 59 [15%]; 1.47, 1.09-1.99) were significantly more common with misoprostol than with oxytocin. Six women had hysterectomies and two women died.
Interpretation Misoprostol is clinically equivalent to oxytocin when used to stop excessive post-partum bleeding suspected to be due to uterine atony in women who have received oxytocin prophylactically during the third stage of labour.
Funding The Bill & Melinda Gates Foundation.
Background Oxytocin, the gold-standard treatment for post-partum haemorrhage, needs refrigeration, intravenous infusion, and skilled providers for optimum use. Misoprostol, a potential alternative, is increasingly used ad hoc for treatment of post-partum haemorrhage; however, evidence is insufficient to lend support to recommendations for its use. This trial established whether sublingual misoprostol is non-inferior to intravenous oxytocin for treatment of post-partum haemorrhage in women receiving prophylactic oxytocin.
Methods In this double-blind, non-inferiority trial, 31 055 women exposed to prophylactic oxytocin had blood loss measured after vaginal delivery at five hospitals in Burkina Faso, Egypt, Turkey, and Vietnam (two secondary-level and three tertiary-level facilities). 809 (3%) women were diagnosed with post-partum haemorrhage and were randomly assigned to receive 800 μg misoprostol (n=407) or 40 IU intravenous oxytocin (n=402). Providers and women were masked to treatment assignment. Primary endpoints were cessation of active bleeding within 20 min and additional blood loss of 300 mL or more after treatment. Clinical equivalence of misoprostol would be accepted if the upper bound of the 97.5% CI fell below the predefined non-inferiority margin of 6%. All outcomes were assessed from the time of initial treatment. This study is registered with ClinicalTrials.gov, number NCT00116350.
Findings All randomly assigned participants were analysed. Active bleeding was controlled within 20 min after initial treatment for 363 (89%) women given misoprostol and 360 (90%) given oxytocin (relative risk [RR] 0.99, 95% CI 0.95-1.04; crude difference 0.4%, 95% CI -3.9 to 4.6). Additional blood loss of 300 mL or greater after treatment occurred for 139 (34%) women receiving misoprostol and 123 (31%) receiving oxytocin (RR 1.12, 95% CI 0.92-1.37). Shivering (152 [37%] vs 59 [15%]; RR 2.54, 95% CI 1.95-3.32) and fever (88 [22%] vs 59 [15%]; 1.47, 1.09-1.99) were significantly more common with misoprostol than with oxytocin. Six women had hysterectomies and two women died.
Interpretation Misoprostol is clinically equivalent to oxytocin when used to stop excessive post-partum bleeding suspected to be due to uterine atony in women who have received oxytocin prophylactically during the third stage of labour.
Funding The Bill & Melinda Gates Foundation.
Post-partum haemorrhage is one of the main contributors to maternal morbidity and mortality worldwide. WHO recommends the administration of a uterotonic agent during active management of the third stage of labour to reduce post-partum bleeding,1 but even with prophylaxis, some women will excessively bleed after childbirth.2 Although oxytocin is regarded as the gold standard for treatment of post-partum haemorrhage,3 misoprostol, a prostaglandin E1 that induces uterine contractions, has been proposed as a low-cost, easy-to-use alternative.4,5 Before this trial, evidence lending support to misoprostol for treatment of post-partum haemorrhage was weak,5-7 and few randomised trials had been done. Nevertheless, misoprostol is being incorporated in clinical services and, in the absence of evidence documenting optimum regimens, providers worldwide are using it ad hoc to stop post-partum bleeding.
The goal of this trial was to establish whether 800 μg sublingual misoprostol is non-inferior to 40 IU oxytocin delivered intravenously for treatment of primary post-partum haemorrhage due to suspected uterine atony in women who have received prophylactic oxytocin during the third stage of labour. A non-inferiority design was chosen since the study sought to identify whether misoprostol is a viable alternative treatment. A parallel trial was undertaken to compare the same treatments in women not receiving prophylactic oxytocin during labour, and these results are reported separately.8 The purpose of undertaking two trials was to understand whether the treatments might work differently in these two groups of women. The dose and route of misoprostol tested were selected after review of the published literature and guidelines;9,10 as well as pharmacokinetic evidence showing that sublingual administration of misoprostol results in the most rapid absorption, highest serum concentrations, and the highest bioavailability;11 and consultation with international experts. On the basis of this review, the trial team chose to test the highest potentially effective dose of both oxytocin and misoprostol, while taking into account safety issues, such as fever and shivering, associated with misoprostol.
Methods
Study setting and patients
This double-blind, randomised trial, undertaken between August, 2005, and January, 2008, compared 800 Êg sublingual misoprostol with 40 IU oxytocin delivered intravenously in five hospitals in Burkina Faso (one), Egypt (one), Turkey (one), and Vietnam (two). Three were tertiary-level teaching hospitals (Burkina Faso, Egypt, Turkey), two were secondary-level facilities (Vietnam), and all managed the third stage of labour with prophylactic oxytocin, delivered either intravenously or intramuscu larly. Other components of active management of the third stage of labour were recorded for every participant and will be reported separately.
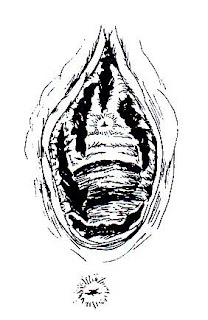
Women were screened for possible inclusion at admission to the labour ward. Written informed consent was obtained in the participant's language. Basic sociodemographic information, haemoglobin concen tration before delivery, and blood loss 1 h post partum were recorded for all screened women. Haemoglobin was measured with a Hemocue device (Hemocue, Angelholm, Sweden), and blood loss was collected in a polyurethane receptacle with a calibrated funnel (Brasss-V Drapes, Excellent Fixable Drapes, Madurai, Tamil Nadu, India), placed under the woman's buttocks after delivery of the baby. Women were excluded if their post-partum haemorrhage was suspected to have a cause other than uterine atony, if oxytocin was not received during the third stage of labour, or if delivery was by caesarean section. Need for treatment was determined by clinical judgment or blood loss reaching 700 mL in the calibrated drape during the first hour after delivery, whichever occurred first.
The protocol was approved by the Western Institutional Review Board (Seattle, WA, USA) and all relevant institutional review boards in participating countries, and is reported in accordance with the revised CONSORT statement.12,13 Continuous monitoring and an independent Data Safety and Monitoring Board (DSMB) ensured protocol adherence. The DSMB reviewed the dataset twice: when two-thirds of cases and 800 cases had been enrolled.
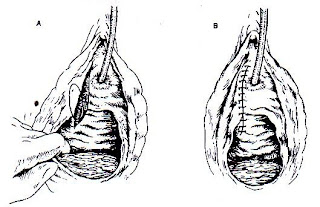
Randomisation and masking
After diagnosis of post-partum haemorrhage, randomisation and treatment occurred immediately. Sealed and numbered opaque boxes contained the treatment allocation and were opened in strict numeric sequence. Participants received simultaneously either 40 IU oxytocin (Boulevard Pharmaceutical Compounding Center, Worcester, MA, USA) in a litre of intravenous solution over 15 min or 800 μg (four tablets of 200 μg) misoprostol (GyMiso, HRA Pharma, Paris, France) placed under the tongue for 20 min and a placebo for the other treatment (ie, four placebo pills or an ampoule of saline). Both providers and women were masked to treatment assignment. A computer-generated random allocation sequence in blocks of ten was derived by Gynuity Health Projects in New York, USA, and was not revealed until data collection and cleaning were completed. Periodic monitoring ensured that hospitals were following the numerical sequence of the boxes and that masking was successful.
Procedures
Blood collection continued for 20 min or until active bleeding stopped, defined as a noticeable slowing in bleeding by clinical assessment, as done in a study on misoprostol for treatment of post-partum haemorrhage in South Africa.14 Measures of blood loss were recorded at time of diagnosis of post-partum haemorrhage, at time of treatment (to capture any delays), 20 min after treatment, and when active bleeding stopped. Measured blood loss could have included blood from episiotomy and other liquids collected during delivery. If active bleeding did not stop within 20 min of initial treatment, providers were instructed to give standard care. Providers were asked to restrict any additional misoprostol to 200 μg in view of the little evidence for this procedure and concerns about high fever and shivering after high doses of misoprostol. After recovery, women were asked about side-effects and accept ability. Haemoglobin concentration after delivery was to be measured no earlier than 12 h after removal of intravenous lines, although this procedure was not always feasible.
Data were collected and recorded by trained staffand reviewed by a designated nurse midwife or physician at every hospital. All forms were translated into local languages and data were entered locally onto a centralised online database developed by Gynuity Health Projects and The Geneva Foundation for Medical Education and Research (Switzerland). Data were available for viewing and cleaning throughout the trial and later transferred for analysis into SPSS (version 15.0).
Statistical analysis
The study was designed as a non-inferiority trial to establish whether misoprostol is a viable alternative treatment for post-partum haemorrhage. Oxytocin was postulated to stop bleeding within 20 min for 88% of women. No trials have been published on the efficacy of oxytocin; therefore its efficacy as the reference treatment was based on expert opinion. It was proposed that misoprostol would work similarly, and that a 6% margin of inferiority (eg, 82%) would be acceptable as clinically equivalent in public health terms. On the basis of these assumptions, for 80% power, á of 0.05, and a one-sided test, 870 women were needed. An additional 10% were planned to account for protocol violations or loss to follow-up for 958 women (479 per group). The primary outcome measures were cessation of active bleeding within 20 min with initial study treatment alone and additional blood loss of 300 mL or more after treatment. Risk difference and 97.5% CI with a one-sided probability were calculated for the primary outcome on which the sample size was calculated: active bleeding stopped within 20 min with initial study treatment. Secondary outcomes were total blood loss after treatment, change in haemoglobin after treatment, time to active bleeding cessation, provision of any additional interventions, and side-effects. All outcomes were assessed from the time of initial treatment per protocol. Stratified analyses by site were undertaken to explore statistical heterogeneity of effect between sites. Comparisons between treatment groups were done and tested for statistical significance with ÷2 tests and Fisher exact test for categorical variables; t tests and Mann-Whitney U tests were used to compare continuous variables. Relative risk (RR) and 95% CIs were calculated as appropriate.
This trial was closed when 809 women had been enrolled. The decision to end the study early was made with advice from the DSMB and expert advisers, after interim analysis showed that none of the primary outcomes had reached significance and showed near-zero probability of reaching even marginal significance. It was therefore determined that non-inferiority had been shown and that the logistical considerations and financial costs of continuing, as well as the public health importance of the results, warranted immediate dissemination of these findings.
This study is registered with ClinicalTrials.gov, number NCT00116350.
Role of the funding source
The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Figure 1 shows the trial profile. Of the 31 055 women screened, 809 (3%) were treated for post-partum haemorrhage with either 800 μg misoprostol sublingually (n=407) or 40 IU oxytocin delivered intravenously (n=402). Baseline characteristics did not differ between the two treatment groups (table 1). All participants diagnosed with post-partum haemorrhage were given the study treatment per protocol. Median blood loss at time of treatment was 700 mL for both groups (table 1).
Active bleeding was controlled within 20 min with the initial treatment for 363 (89%) women receiving misoprostol and 360 (90%) receiving oxytocin (RR 0.99, 95% CI 0.95-1.04), and additional blood loss of 300 mL or more after treatment was recorded for 139 (34%) women receiving misoprostol and 123 (31%) receiving oxytocin (1.12, 0.92-1.37; table 2). Stratified analysis of both primary outcomes by study site showed no differences (data not shown).
The crude overall difference in the proportion of women in the misoprostol versus oxytocin treatment groups whose active bleeding was not controlled within 20 min with initial treatment was 0.4% (95% CI -3.9 to 4.6). This upper confidence limit of the difference of primary interest with the non-inferiority design is within the 6% range stated in the study hypothesis (figure 2). The absolute difference between study groups in percentage of women whose bleeding was not controlled within 20 min ranged from -0.7% to 5.9% across study sites.
Median additional blood loss after treatment did not differ between groups (table 2). There was no difference in additional blood loss of 500 mL or more after treatment (RR 1.09, 95% CI 0.77-1.54) but additional blood loss of 1000 mL or more after treatment was more common with misoprostol than with oxytocin (3.62, 1.02-12.89; table 2). Active bleeding restarted for 13 (3%) of women receiving misoprostol and 12 (3%) receiving oxytocin (p=0.515).
Haemoglobin concentrations after treatment for all women averaged 96 g/L, and mean drop in haemoglobin after delivery did not differ between the two groups (table 2). 152 (37%) women receiving misoprostol versus 142 (35%) receiving oxytocin had a drop in haemoglobin of 20 g/L (RR 1.06, 95% CI 0.88-1.27), of whom 104 (26%) and 90 (22%), respectively, had a drop of 30 g/L or more (1.14, 0.89-1.46).
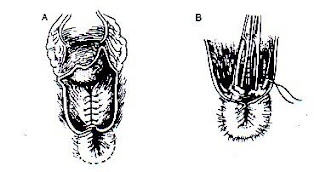
Additional uterotonic drugs were given to 40 (10%) women receiving misoprostol and 46 (11%) receiving oxytocin (RR 0.86, 95% CI 0.58-1.28), and blood transfusions were given to 24 (6%) and 18 (4%) participants, respectively (1.32, 0.73-2.39). Women given misoprostol were more likely to undergo intrauterine exploration under anaesthesia than were those given oxytocin (RR 1.66 95% CI 1.00-2.76; table 2). Other interventions, including bimanual compression and hysterectomy, were infrequent (table 2).
Side-effects were noted for all participants (table 3). Shivering and fever were recorded significantly more often in women allocated to misoprostol than in those allocated to oxytocin (table 3). Reports of other side-effects and their tolerability did not differ significantly between the two groups (table 2) and none resulted in extended stay in hospital. Most women (>90%) reported being either satisfied or neutral with the modes of treatment administration (eg, pills under tongue or tube in arm; data not shown).
Serious adverse events were reported for seven participants and included six hysterectomies (four with misoprostol and two with oxytocin). Two of these women died of uncontrolled post-partum bleeding. One woman allocated to oxytocin had severe atonic post-partum haemorrhage that was unresponsive to treatment, had cardiac arrest twice during hysterectomy, and later died; the second woman allocated to misoprostol had disseminated intravascular coagulation, severe anaemia, and signs of shock after delivery. Hysterectomy was done, but she died the next day. A suspected allergic reaction was also reported for one participant allocated to misoprostol. The symptoms disappeared within 3 h and the woman was discharged in good health.
Discussion
Researchers and policy makers have been enthusiastic about misoprostol as treatment for post-partum haemorrhage, but evidence to support a particular regimen has been scarce.7,15 These findings provide evidence that 800 μg sublingual misoprostol is a viable alternative to 40 IU intravenous oxytocin for treatment of primary post-partum haemorrhage after oxytocin prophylaxis during the third stage of labour. Misoprostol stopped bleeding as rapidly as did oxytocin and with a similar quantity of additional blood loss. Although rare for both groups, women given misoprostol were more likely to bleed an additional 1000 mL or more than were those given oxytocin.
The crude overall difference in the proportion of women whose active bleeding was not controlled within 20 min with initial treatment or post-partum haemorrhage was within the prespecified 6% margin of non-inferiority. Availability, cost, ease of administration, and feasibility could also affect the choice of treatment. For providers and policy makers concerned about the fever and chills associated with misoprostol, treatment with oxytocin might be preferable. Misoprostol, however, has several advantages that could affect treatment policy recommendations in the future: the tablets can be quickly administered at the place of delivery by placing them under a woman's tongue, can be stored for several years at ambient temperatures in sealed blister packets, and can be offered by providers who are not trained or authorised to administer intravenous infusions. Indeed, oxytocin might be associated with delays in treatment while the intravenous lines are inserted or providers who are trained to do so are located. In some circumstances, misoprostol might be the only treatment option-eg, when deliveries are mostly undertaken by health-care workers who are trained and authorised only to administer drugs intramuscularly. In these situations, misoprostol treatment could reduce the need for transfer to higher-level facilities and decrease the workload for skilled providers at referral centres. Since about 10% of women will need additional treatment for post-partum haemorrhage, systems should be in place for timely referral to higher-level care.
Serious side-effects after treatment were uncommon; however, misoprostol was associated with more fevers and shivering than was oxytocin. Five women given misoprostol had temperatures of 40.0°C or higher compared with one woman given oxytocin. The occurrence of fever after misoprostol administration for post-partum haemorrhage is well documented. Four cases of temperatures of 40.0°C or higher have been reported after treatment for post-partum haemorrhage with doses of 600 μg or 1000 μg misoprostol.6,16 Although none of the fevers in this trial needed additional interventions, providers should be trained to identify and manage high fever.
Before this trial, evidence lending support to misoprostol for treatment of post-partum haemorrhage was scarce.5-7,15 A PubMed review of reports on misoprostol for post-partum haemorrhage treatment published in English or French up to March, 2009, found four randomised controlled trials on this topic.14,16-18 Three reported on misoprostol as an adjunct to standard treatments for post-partum haemorrhage.16-18 Lokugamage and colleagues14 reported that 800 μg rectal misoprostol conferred a significant advantage compared with ergometrine plus oxytocin and intravenous oxytocin for treatment of post-partum haemorrhage. However, the study was not masked and blood loss was assessed visually, which could have led to investigator bias. Eight other reports tested a range of misoprostol doses (200-1000 μg) and routes of administration.19-27 These studies offer little evidence to lend support to a specific treatment regimen. Two reviews concluded that there is insufficient evidence to lend support to misoprostol for treatment of post-partum haemorrhage.5,7
This trial has limitations. As with all clinical trials, the study environment alone could have affected outcomes at participating hospitals. However, since both providers and women were not aware of study treatment, environment should have little effect on the efficacy comparisons. Further, since no randomised studies have established the efficacy of oxytocin for treatment of post-partum haemorrhage, it is conceivable that neither treatment is much better than no uterotonic treatment. This issue will probably never be addressed in view of the impossibility of offering no treatment to a haemorrhaging patient.
Because of the potential for pyrexia after misoprostol use, concerns have been raised about the safety of misoprostol when administered as both prophylaxis and treatment. 7 After Derman and colleages28 reported a 50% reduction in occurrence of post-partum haemorrhage (blood loss .500 mL) in women given 600 Êg oral misoprostol prophylactically,28 some countries have adopted pro gram mes promoting universal prevention with misoprostol. Yet, very little is known about treatment for post-partum haemorrhage in women given misoprostol prophylactic ally in the third stage of labour, and whether treatment with misoprostol would be as effective for these women is uncertain. In the absence of clinical data exploring outcomes when the drug is administered for both prevention and treatment, provider training and service-delivery guidelines should emphasise close monitoring of patients to ensure the best maternal outcomes. Additional information might be needed for programmes considering simultaneous introduction of misoprostol for both prevention and treatment of post-partum haemorrhage.
This trial reports on misoprostol and oxytocin use for post-partum haemorrhage in women who received prophylactic oxytocin. The results of another, similar, trial in women not receiving oxytocin prophylactically are reported separately.8 In the other trial, both oxytocin and misoprostol were more effective in stopping bleeding within 20 min than they were in this trial, with oxytocin being significantly more effective in that trial (95% for oxytocin vs 90% for misoprostol in the other trial compared with the 90% vs 89% efficacy in this trial). In women treated for post-partum haemorrhage who had not received oxytocin in the third stage of labour, oxytocin and misoprostol were both effective, but all primary and secondary outcomes significantly favoured oxytocin. Although haemorrhage occurred in fewer women given oxytocin prophylactically in the third stage of labour, haemorrhage in this group of women seemed to be more serious and more resistant to treatment. Time to bleeding cessation was on average faster (12 min) for women with a previously untreated uterus in the concurrent trial, compared with 19 min in this trial. Oxytocin seemed to perform less well in women in this study than in those who haemorrhaged without prophylaxis. Perhaps women who bleed excessively after oxytocin are a special subgroup, in some way resistant to the uterotonic effects of that drug and, for them, oxytocin provides less treatment benefit than for the population as a whole. In this subgroup of women the usual advantages of oxytocin over misoprostol, even if small, are effectively erased.
Although international momentum lending support to the introduction of misoprostol programmes for post-partum haemorrhage has grown, some questions remain that could affect service delivery. Future research should investigate the effectiveness of treatment for post-partum haemorrhage with misoprostol when introduced widely into clinical practice at secondary and primary health-care facilities and, importantly, after misoprostol prophylaxis has been administered. Clinical research examining whether a lower treatment dose shows similar effectiveness with fewer undesirable side-effects would also be useful. Service-delivery guidelines tailored to providers at all levels should be developed to improve management of post-partum haemorrhage with all available methods.
Contributors
JB, BW, and RD contributed to the conception of the trial. BW, JB, RD, MCR, and NTNN participated in the study design. All authors participated in the study implementation, data analysis, and interpretation of results. JB, SR, and JD drafted the report with input and editing from all authors.
Conflicts of interest
We declare that we have no conflicts of interest.
Acknowledgments
We thank the women who participated in this trial and the providers who carefully collected the data; our colleagues at Family Care International; the members of our Post-Partum Haemorrhage Advisory Committee: Paul Blumenthal, Jose Guilherme Cecatti, Friday Okonofua, Swaraj Rajbhandari, Nancy Sloan, JeffSpieler, and Gijs Walraven; the Data Safety and Monitoring Board Members: Jose Guilherme Cecatti, Thomas Easterling, and Anne Paxton for their contributions to this trial; Nevine Hassanein, Abdel Aziz El Shobary, and Miral Breebaart in Egypt; Ngo Van Nhang at Hoc Mon Hospital and Tran Thanh Nhan at Cu Chi Hospital in Vietnam; Der Adolphe Somé and Pascaline Zongo Tamini at Centre Hospitalier Souro Sanou in Burkina Faso; Ali Haberal, Salim Erkaya, Omer Kandemir, Dilek Torun, and Nurten Kaya at MoH Etlik Zubeyde Hanim Women's Health Teaching and Research Hospital in Turkey; and Melanie Peña at Gynuity Health Projects. This research was funded by a grant from the Bill & Melinda Gates Foundation.
Sidebar
References
References
1 WHO. Recommendations for the prevention of postpartum haemorrhage. Department of Making Pregnancy Safer. Geneva: World Health Organization, 2007.
2 Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev 2000; 3: CD000007.
3 WHO. Managing complications in pregnancy and childbirth: a guide for midwives and doctors. Geneva: Department of Reproductive Health and Research, World Health Organization, 2000.
4 Tsu VD, Shane B. New and underutilized technologies to reduce maternal mortality: call to action from a Bellagio workshop. Int J Gynaecol Obstet 2004; 85 (suppl 1): S83-93.
5 Mousa HA, Alfirevic Z. Treatment for primary postpartum haemorrhage. Cochrane Database Syst Rev 2007; 1: CD003249.
6 Hofmeyr GJ, Walraven G, Gülmezoglu AM, Alfirevic Z, Villar J. Misoprostol to treat postpartum hemorrhage: a systematic review. BJOG 2005; 112: 547-53.
7 Blum J, Alfirevic Z, Walraven G, Weeks A, WinikoffB. Treatment of postpartum hemorrhage with misoprostol. Int J Gynaecol Obstet 2007; 99 (suppl 2): 202-05.
8 WinikoffB, Dabash R, Durocher J, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labour: a double-blind, randomised, non-inferiority trial. Lancet 2010; published online Jan 7. DOI:10.1016/S0140-6736(09)61924-3.
9 American College of Obstetricians and Gynaecologists. ACOG practice bulletin: clinical management guidelines for obstetrician-gynecologists number 76, October 2006: postpartum haemorrhage. Obstet Gynecol 2006; 108: 1039-47.
10 Royal College of Obstetricians and Gynaecologists. Prevention and management of postpartum haemorrhage. RCOG green-top guideline. number 52. London: Royal College of Obstetricians and Gynaecologists, 2009.
11 Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet 2007;99 (suppl 2): S160-67.
12 Altman DG, Schulz KF, Moher D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 2001; 134: 663-94.
13 Piaggio G, Elbourne D, Altman D, Pocock S, Evans S. Reporting of noninferiority and equivalence randomised trials: an extension of the CONSORT statement. JAMA 2006; 295: 1152-60.
14 Lokugamage AU, Sullivan KR, Niculescu I, et al. A randomized study comparing rectally administered misoprostol versus Syntometrine combined with an oxytocin infusion for the cessation of primary post partum hemorrhage. Acta Obstet Gynecol Scand 2001; 80: 835-39.
15 Hofmeyr GJ, Gulmezoglu AM. Misoprostol for the prevention and treatment of postpartum haemorrhage. Best Pract Res Clin Obstet Gynaecol 2008; 22: 1025-41.
16 Zuberi N, Durocher J, Sikander R, Baber N, Blum J, Walraven G. Misoprostol in addition to routine treatment of postpartum hemorrhage: a hospital-based randomized controlled-trial in Karachi, Pakistan. BMC Pregnancy Childbirth 2008; 8: 40.
17 Hofmeyr GJ, Ferreira S, Nikodem VC, et al. Misoprostol for treating postpartum hemorrhage: a randomized controlled trial. BMC Pregnancy Childbirth 2004; 4: 16.
18 Walraven G, Dampha Y, Bittaye B, Sowe M, Hofmeyr J. Misoprostol in the treatment of postpartum haemorrhage in addition to routine management: a placebo randomized controlled trial. BJOG 2004; 111: 1014-17.
19 Mousa HA, Alfirevic Z. Treatment for primary postpartum haemorrhage. Cochrane Database of Systematic Reviews 2007; 1: CD003249.
20 O'Brien P, El-Refaey H, Gordon A, Geary M, Rodeck CH. Rectally administered misoprostol for the treatment of postpartum hemorrhage unresponsive to oxytocin and ergometrine: a descriptive study. Obstet Gynecol 1998, 92: 212-14.
21 Ozan H, Bilgin T, Ozsarac N, Ozerkan RK, Cengiz C. Misoprostol in uterine atony: a report of 2 cases. Clin Exp Obstet Gynecol 2000; 27: 221-22.
22 Abdel-aleem H, El-Nashar I, Abdel-Aleem A. Management of severe postpartum hemorrhage with misoprostol. Int J Gynaecol Obstet 2001; 72: 75-76.
23 Shojai R, Debriere R, Dhifallah S, et al. [Rectal misoprostol for postpartum hemorrhage.] Gynecol Obstet Fertil 2004; 32: 703-07.
24 Shojai R, Piechon L, d'Ercole C, Boubli L, Ponties JE. [Rectal administration of misoprostol for delivery induced hemorrhage. Preliminary study.] J Gynecol Obstet Reprod Biol 2001; 30: 572-75.
25 Adekanmi OA, Purmessur S, Edwards G, Barrington JW. Intrauterine misoprostol for the treatment of severe recurrent atonic secondary postpartum haemorrhage. BJOG 2001; 108: 541-45.
26 Oboro VO, Tabowei TO, Bosah JO. Intrauterine misoprostol for refractory postpartum hemorrhage. Int J Gynaecol Obstet 2003; 80: 67-68.
27 Prata N, Mbaruku G, Campbell M, Potts M, Vahidnia F. Controlling postpartum hemorrhage after home births in Tanzania. Int J Gynaecol Obstet 2005; 90: 51-55.
28 Derman RJ, Kodkany BS, Goudar SS, et al. Oral misoprostol in preventing postpartum haemorrhage in resource-poor communities: a randomised controlled trial. Lancet 2006; 368: 1248-53.
1 WHO. Recommendations for the prevention of postpartum haemorrhage. Department of Making Pregnancy Safer. Geneva: World Health Organization, 2007.
2 Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev 2000; 3: CD000007.
3 WHO. Managing complications in pregnancy and childbirth: a guide for midwives and doctors. Geneva: Department of Reproductive Health and Research, World Health Organization, 2000.
4 Tsu VD, Shane B. New and underutilized technologies to reduce maternal mortality: call to action from a Bellagio workshop. Int J Gynaecol Obstet 2004; 85 (suppl 1): S83-93.
5 Mousa HA, Alfirevic Z. Treatment for primary postpartum haemorrhage. Cochrane Database Syst Rev 2007; 1: CD003249.
6 Hofmeyr GJ, Walraven G, Gülmezoglu AM, Alfirevic Z, Villar J. Misoprostol to treat postpartum hemorrhage: a systematic review. BJOG 2005; 112: 547-53.
7 Blum J, Alfirevic Z, Walraven G, Weeks A, WinikoffB. Treatment of postpartum hemorrhage with misoprostol. Int J Gynaecol Obstet 2007; 99 (suppl 2): 202-05.
8 WinikoffB, Dabash R, Durocher J, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labour: a double-blind, randomised, non-inferiority trial. Lancet 2010; published online Jan 7. DOI:10.1016/S0140-6736(09)61924-3.
9 American College of Obstetricians and Gynaecologists. ACOG practice bulletin: clinical management guidelines for obstetrician-gynecologists number 76, October 2006: postpartum haemorrhage. Obstet Gynecol 2006; 108: 1039-47.
10 Royal College of Obstetricians and Gynaecologists. Prevention and management of postpartum haemorrhage. RCOG green-top guideline. number 52. London: Royal College of Obstetricians and Gynaecologists, 2009.
11 Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet 2007;99 (suppl 2): S160-67.
12 Altman DG, Schulz KF, Moher D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 2001; 134: 663-94.
13 Piaggio G, Elbourne D, Altman D, Pocock S, Evans S. Reporting of noninferiority and equivalence randomised trials: an extension of the CONSORT statement. JAMA 2006; 295: 1152-60.
14 Lokugamage AU, Sullivan KR, Niculescu I, et al. A randomized study comparing rectally administered misoprostol versus Syntometrine combined with an oxytocin infusion for the cessation of primary post partum hemorrhage. Acta Obstet Gynecol Scand 2001; 80: 835-39.
15 Hofmeyr GJ, Gulmezoglu AM. Misoprostol for the prevention and treatment of postpartum haemorrhage. Best Pract Res Clin Obstet Gynaecol 2008; 22: 1025-41.
16 Zuberi N, Durocher J, Sikander R, Baber N, Blum J, Walraven G. Misoprostol in addition to routine treatment of postpartum hemorrhage: a hospital-based randomized controlled-trial in Karachi, Pakistan. BMC Pregnancy Childbirth 2008; 8: 40.
17 Hofmeyr GJ, Ferreira S, Nikodem VC, et al. Misoprostol for treating postpartum hemorrhage: a randomized controlled trial. BMC Pregnancy Childbirth 2004; 4: 16.
18 Walraven G, Dampha Y, Bittaye B, Sowe M, Hofmeyr J. Misoprostol in the treatment of postpartum haemorrhage in addition to routine management: a placebo randomized controlled trial. BJOG 2004; 111: 1014-17.
19 Mousa HA, Alfirevic Z. Treatment for primary postpartum haemorrhage. Cochrane Database of Systematic Reviews 2007; 1: CD003249.
20 O'Brien P, El-Refaey H, Gordon A, Geary M, Rodeck CH. Rectally administered misoprostol for the treatment of postpartum hemorrhage unresponsive to oxytocin and ergometrine: a descriptive study. Obstet Gynecol 1998, 92: 212-14.
21 Ozan H, Bilgin T, Ozsarac N, Ozerkan RK, Cengiz C. Misoprostol in uterine atony: a report of 2 cases. Clin Exp Obstet Gynecol 2000; 27: 221-22.
22 Abdel-aleem H, El-Nashar I, Abdel-Aleem A. Management of severe postpartum hemorrhage with misoprostol. Int J Gynaecol Obstet 2001; 72: 75-76.
23 Shojai R, Debriere R, Dhifallah S, et al. [Rectal misoprostol for postpartum hemorrhage.] Gynecol Obstet Fertil 2004; 32: 703-07.
24 Shojai R, Piechon L, d'Ercole C, Boubli L, Ponties JE. [Rectal administration of misoprostol for delivery induced hemorrhage. Preliminary study.] J Gynecol Obstet Reprod Biol 2001; 30: 572-75.
25 Adekanmi OA, Purmessur S, Edwards G, Barrington JW. Intrauterine misoprostol for the treatment of severe recurrent atonic secondary postpartum haemorrhage. BJOG 2001; 108: 541-45.
26 Oboro VO, Tabowei TO, Bosah JO. Intrauterine misoprostol for refractory postpartum hemorrhage. Int J Gynaecol Obstet 2003; 80: 67-68.
27 Prata N, Mbaruku G, Campbell M, Potts M, Vahidnia F. Controlling postpartum hemorrhage after home births in Tanzania. Int J Gynaecol Obstet 2005; 90: 51-55.
28 Derman RJ, Kodkany BS, Goudar SS, et al. Oral misoprostol in preventing postpartum haemorrhage in resource-poor communities: a randomised controlled trial. Lancet 2006; 368: 1248-53.